Can Human Milk Sugars Help Soothe IBS? Exploring the Gut Microbiome’s Sweet Spot
The Paper of the Month for June is ‘An in vitro batch culture study to assess the fermentation of human milk oligosaccharides by faecal microbiota from healthy and irritable bowel syndrome stool donors‘. The blog is written by author Patricia Sanz Morales et al, and the paper is published in the Gut Microbiome.
If you’ve ever cared for a baby, you might know that human milk contains more than just nutrients—it’s packed with complex sugars called human milk oligosaccharides (HMOs). These aren’t digestible by infants but serve as food for beneficial gut bacteria, helping to shape a healthy microbiome from day one.
But here’s the twist: could these same sugars help adults with gut issues like Irritable Bowel Syndrome (IBS)? A recent study led by researchers at The University of Reading suggests they might.
The Gut Microbiome and IBS
IBS affects up to 15% of people worldwide and is often linked to an imbalance in gut bacteria, known as dysbiosis. People with IBS typically have lower levels of beneficial bacteria like Bifidobacterium and Faecalibacterium, along with reduced production of short-chain fatty acids (SCFAs)—compounds that support gut health.
The Study: Feeding Gut Bacteria with HMOs
In this study, researchers used an in vitro (lab-based) system to simulate the human gut environment. They collected stool samples from both healthy individuals and those with IBS, then introduced various HMOs to see how the gut bacteria would respond.

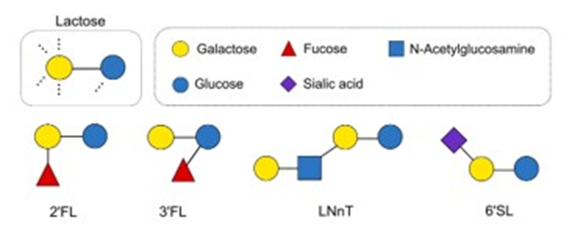
The HMOs tested included:
- 2′-fucosyllactose (2′FL)
- 3′-fucosyllactose (3′FL)
- 3′-sialyllactose (3′SL)
- 6′-sialyllactose (6′SL)
- Lacto-N-tetraose (LNT)
- Lacto-N-neotetraose (LNnT)
- Mixes of 2′FL/3′SL and 3′SL/LNT
Key Findings
- Baseline Differences: IBS samples started with different microbial profiles compared to healthy ones, notably lower levels of beneficial bacteria and SCFAs.
- Positive Response to HMOs: After introducing HMOs, both healthy and IBS samples showed changes in their microbiomes. Notably, IBS samples experienced significant increases in Bifidobacterium and Faecalibacterium populations, as well as higher SCFA production.
- Top Performer: Among the HMOs tested, the combination of 3′SL and LNT was particularly effective in promoting beneficial bacterial growth and SCFA production in IBS samples.
Why This Matters
These findings suggest that HMOs could serve as prebiotics—compounds that feed beneficial gut bacteria—in adults with IBS. By enhancing the growth of good bacteria and boosting SCFA levels, HMOs might help alleviate some IBS symptoms.
It’s important to note that this was an in vitro study, meaning it was conducted outside the human body. While the results are promising, clinical trials are necessary to confirm the benefits of HMOs for IBS patients in real-world settings.
Looking Ahead
The idea of using components from human milk to support adult gut health is both innovative and grounded in our understanding of the microbiome. As research progresses, HMOs could become a valuable tool in managing IBS and perhaps other gut-related conditions.
For those interested in the nitty-gritty details, you can access the full study here: An in vitro batch culture study to assess the fermentation of human milk oligosaccharides by faecal microbiota from healthy and irritable bowel syndrome stool donors.